What is a Spinal Compression Fracture?
Not the same as a fracture, such as in an arm when a person falls awkwardly on it, a spinal compression fracture is usually defined as a vertebral bone in the spine that has decreased at least 15 to 20 percent in height due to fracture.
This usually occurs in vertebrae that have been weakened by osteoporosis or other diseases that weaken bone, such as cancer. The fracture occurs when the bone has deteriorated to the degree that it can no longer support the spinal column and the daily loads placed upon the vertebrae. You can think of the vertebrae as cracking like an overstressed piece of concrete.
Where do Spinal Compression Fractures typically occur?
Most compression fractures occur in the thoracic region of the spine or the lumbar spine. The thoracic spine is the center of the spine between the cervical (neck) region and the lumbar (lower back) region. The thoracic spine includes 12 vertebrae, T1 through T12. The lumbar spine is the bottom of the spine, vertebra L1 through L5, where it enters the hips.
What are the symptoms of a Spinal Compression Fracture?
Symptoms can vary. Sometimes, if the compression is just beginning to crack the bone, the patient may not have symptoms. In most cases, however, the fracture results in a wedge-shaped vertebra, as the bone in the front of the spinal column collapses and loses height, but the back of the bone remains unchanged and at the same original height. Symptoms may include:
- Severe acute back pain that feels better when the patient lies down
- Pain in the back, arms, or legs
- Numbness and/or weakness in the arms or legs (if the fracture has affected the spinal cord or the surrounding nerve roots)
- Loss of height
- Hunched forward position (kyphosis)
What causes Spinal Compression Fractures, and who is at risk?
The typical cause of these fractures is osteoporosis, a condition that causes the bones to lose mass, and become weak and brittle. Osteoporosis is most common in elderly women, and this is the group most at risk.
Far less frequently, this can occur in patients whose vertebrae have been weakened by a tumor or infection.
Even more infrequently, compression fractures can result from trauma.
How are Spinal Compression Fractures diagnosed?
After a physical examination and discussion of the patient’s medical history, imaging tests are used to confirm diagnoses:
- X-rays: X-rays provide an overall assessment of the bone anatomy, as well as the curvature and alignment of the vertebral column. Spinal dislocation or slippage, kyphosis, scoliosis, and overall spine balance can be assessed with x-rays. Bone spurs and disc space narrowing will also show up.
- Magnetic resonance imaging (MRI): MRIs use large magnets, radiofrequency energy, and a computer to produce detailed images of the structures. They show soft tissue, where x-rays do not.
- Computerized tomography (CT Scan): CT scans produce detailed images of any part of the body, including the bones, muscles, fat, and organs.
- Nuclear bone scan: A radioactive substance is injected into the body to measure the activity in the bones. This material then shows up on the scan, detailing damaged areas.
How is a Spinal Compression Fracture treated?
Treatment for spinal compression fractures due to osteoporosis usually has two aspects: treating the fracture and treating the underlying osteoporosis.
Fracture Treatment
Non-surgical treatments are often recommended for these spinal fractures. This includes pain medications and modifying the patient’s physical activity to try and allow the fracture to heal. A brace can help to support the back, preventing the person from bending forward, which removes pressure from the fractured vertebrae. These fractures can heal in about three months.
Treatment for Osteoporosis
Treating the osteoporosis has the goal of preventing future compression fractures. These treatments seek to help rebuild bone mass, or to at least stop the bone loss. Treatments include calcium and vitamin D supplements, bisphosphonates, and weight-bearing exercise.
When is surgery used?
Dr. Michael Turner may be called on to perform surgery when the spine appears to be unstable. Two procedures are used:
Vertebroplasty
This is a minimally invasive procedure where low-viscosity bone cement is injected directly into the collapsed vertebra under high pressure. The goal is to stabilize the fracture and relieve the associated pain.
Kyphoplasty
This is similar to vertebroplasty, except that a balloon is first inserted into the vertebral body and is inflated. This raises the collapsed vertebra back up to its former height, creating a cavity into which Dr. Turner can then inject the bone cement under lower pressure.
This fills the cavity and returns strength to the vertebra. The procedure may be repeated on the other side of the vertebra to ensure the cavity is evenly filled. The goal with kyphoplasty is to regain height in the collapsed vertebra.
What is the recovery process from a Spinal Compression Fracture?
When non-surgical approaches are used, the patient’s pain is managed with medication and physical activity is limited to allow the fracture to heal. This takes about three months.
In kyphoplasty and vertebroplasty, the bone cement fully hardens in as little as five minutes. Patients can return home the same day. Pain relief is usually immediate. At home, patients can return to their normal daily activities quickly.
Strenuous exertion, especially heavy lifting, needs to be avoided for six weeks. Otherwise, patients can return to most normal activities and easier forms of exercise after just a couple days. A physical therapist will likely be involved and will show you exercises to help you recover. These will also help with the weight-bearing exercise needed to strengthen bones weakened by osteoporosis.
Comprehensive Neurosurgery Reviews
"Dr. Turner and his staff are awesome folks.They took great care of me."
"Everything is great, the staff, nurses, and Dr. Turner. From preoperative care, to the surgery, and postoperative care. All my questions were answered, concerns, and care was excellent. I would recommend him to anyone and everyone that might need surgery on their back."
"As a new patient, Dr Turner and his staff have given me confidence that my surgical issues will be handled and that the best results will be achieved."
Schedule Your Spinal Fracture Consultation Today!
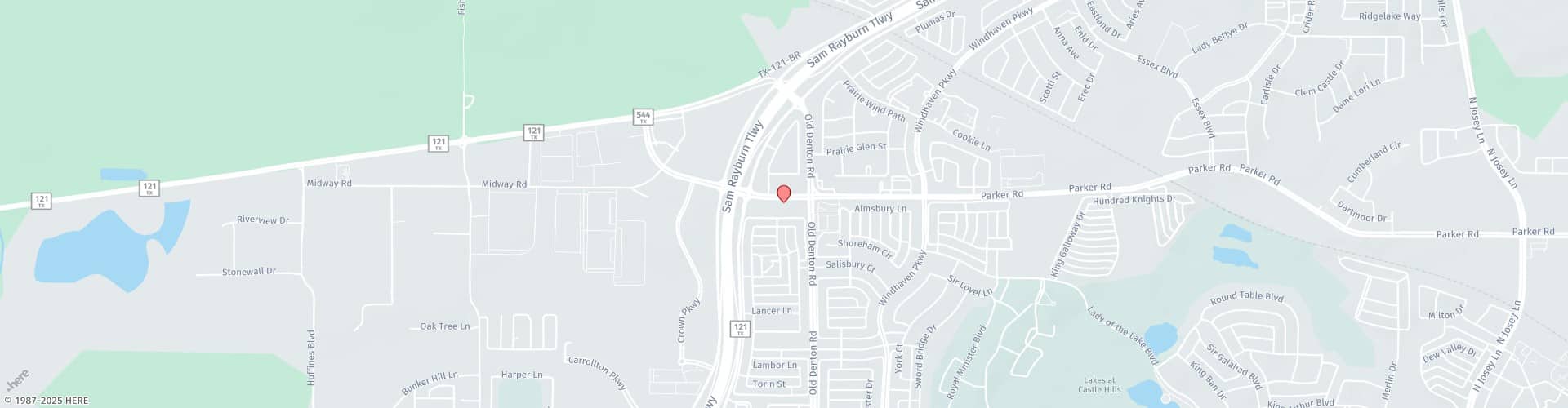
Please call 972.394.4600 to schedule your consultation with Dr. Michael Turner today! Our practice serves Lewisville, TX & the greater Dallas area.